Landmark 2025 Agreement Redefines Pandemic Response and Vaccine Access
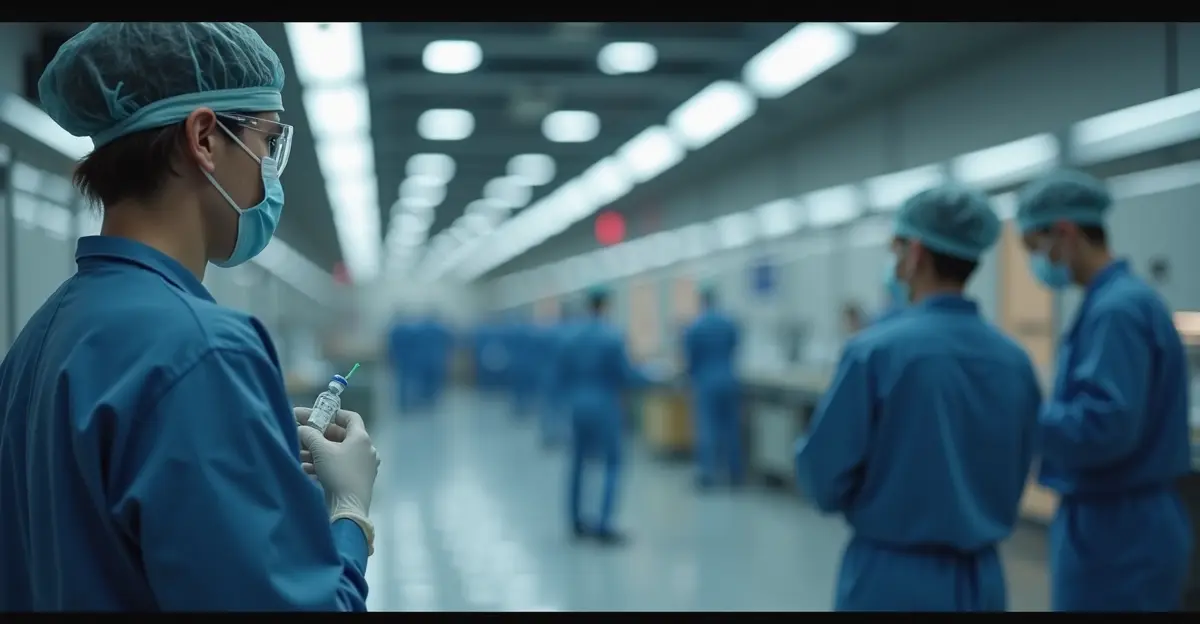
The global health landscape underwent a seismic shift in May 2025 when the World Health Assembly adopted a historic Pandemic Agreement that fundamentally transforms how vaccines and medical technologies are shared worldwide. This landmark deal, years in the making, directly addresses the vaccine inequity that plagued the COVID-19 response, where wealthy nations secured early access while developing countries waited months for life-saving doses.
The Core of the Agreement: Technology Transfer as a Right
At the heart of the agreement lies a revolutionary approach to technology transfer. For the first time in global health governance, there are explicit obligations for states to promote the transfer of vaccine technologies to developing countries. The agreement establishes WHO's Health Technology Access Programme as a central mechanism for facilitating these transfers, moving beyond the charity-based models that dominated previous pandemic responses.
'This isn't just about sharing formulas—it's about building sustainable capacity where it's needed most,' explains Dr. Maria Rodriguez, a global health policy expert at Johns Hopkins University. 'The agreement recognizes that true equity means enabling countries to produce their own solutions rather than waiting for handouts.'
The mRNA Technology Transfer Programme: A Blueprint for Success
Running parallel to the broader agreement is WHO's mRNA Technology Transfer (mRNA TT) Programme, which has been operational since 2021 but gained new momentum with the 2025 framework. This initiative has established regional mRNA vaccine production hubs across Africa, South America, and Asia, with thirteen program partners across Argentina, Bangladesh, Brazil, Egypt, and India already signing technology transfer agreements.
The program represents a strategic investment in local manufacturing capabilities. Afrigen in South Africa serves as the global mRNA technology development center, while Biovac is scaling up production capabilities. These hubs aren't just manufacturing facilities—they're centers of innovation and knowledge transfer that will strengthen regional health security for decades to come.
Market Implications and Economic Shifts
The technology transfer deal is already reshaping global pharmaceutical markets. Traditional vaccine manufacturers are adapting to a new landscape where production is more geographically distributed. While some industry analysts initially expressed concerns about intellectual property protections, the agreement's careful language has addressed many of these worries.
'The compromise language around 'mutually agreed terms' was crucial,' notes pharmaceutical policy analyst James Chen. 'It preserves intellectual property rights while creating pathways for voluntary technology sharing. This balanced approach makes the agreement workable for both innovators and those needing access.'
The agreement explicitly states that technology transfer should occur "as mutually agreed," defined in a footnote as "willingly undertaken and on mutually agreed terms, without prejudice to the rights and obligations of the Parties under other international agreements." This careful wording maintains the delicate balance between innovation incentives and public health needs.
Community Impact and Local Empowerment
For communities in developing regions, the implications are profound. The WHO Africa and International Vaccine Institute (IVI) recently signed a landmark Memorandum of Understanding to strengthen vaccine equity, local production, and health innovation across Africa. This partnership aims to build Africa's capacity in vaccine research, development, and manufacturing for what officials call "health sovereignty."
'We're moving from being recipients to becoming producers and innovators,' says Dr. Amina Bello, a public health official in Nigeria. 'This isn't just about pandemic response—it's about building resilient health systems that can address local health challenges year-round.'
The technology transfer approach addresses the estimated one million preventable deaths from COVID-19 vaccine inequity by creating more distributed manufacturing networks. When the next pandemic strikes—and experts agree it's a matter of when, not if—these regional production hubs will enable faster, more equitable responses.
Implementation Challenges and Future Outlook
Despite the agreement's ambitious goals, implementation challenges remain. Building sustainable manufacturing capacity requires not just technology transfer but also regulatory harmonization, workforce development, and quality control systems. The agreement addresses these through provisions for regulatory authority strengthening and workforce development in vaccinology.
The Pandemic Agreement enters into force 30 days after 60 countries ratify it, with implementation overseen by a Conference of the Parties. This governance structure ensures ongoing monitoring and adaptation as the global health landscape evolves.
As the world continues to grapple with the lessons of COVID-19, this 2025 technology transfer deal represents more than just policy—it's a fundamental rethinking of how global health equity can be achieved. By shifting from charity to capacity building, from centralized production to distributed networks, and from temporary solutions to sustainable systems, the agreement offers hope for a more equitable future in global health.
For more information on the WHO Pandemic Agreement, visit WHO's official page. Details about the mRNA Technology Transfer Programme are available at WHO's mRNA TT Programme.

 Nederlands
Nederlands
 English
English
 Deutsch
Deutsch
 Français
Français
 Español
Español
 Português
Português