Telemedicine Trials Launch in Rural Regions
New telemedicine trials are launching in rural regions worldwide, aiming to address healthcare access disparities through remote diagnostics. These initiatives enable real-time consultations with specialists, remote patient monitoring, and AI-assisted diagnostics. For example, telecardiology programs in the Midwest U.S. have reduced stroke treatment delays from hours to minutes by enabling "golden hour" interventions. Similar programs in Nepal use AI-powered retinal scans to detect diabetic retinopathy with 98.57% sensitivity.
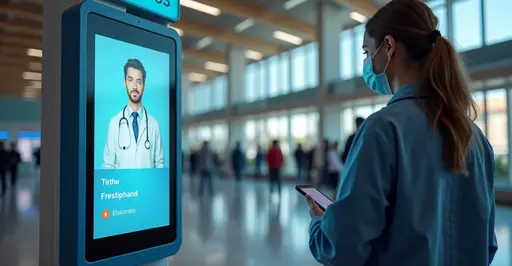
How Remote Diagnostics Work
Using IoT devices and mobile applications, patients in remote areas can now:
- Transmit vital signs to specialists in real-time
- Receive AI-powered preliminary diagnoses
- Access specialist consultations via video conferencing
- Use store-and-forward technology for non-urgent cases
A recent systematic review found telehealth reduced unnecessary patient transfers by 37% in critical access hospitals.
Overcoming Implementation Barriers
Despite promising results, challenges remain:
- Infrastructure: 24% of rural areas lack broadband meeting telehealth requirements
- Costs: Setup ranges from $17,000-$50,000 with $60,000+ annual subscriptions
- Training: New Mexico's "Telehealth Frontier" program shows clinician training boosts adoption by 68%
Policy solutions include revised Medicare reimbursement models and regional telehealth networks like the Great Plains Telehealth Resource Center.
Future Outlook
Ongoing trials focus on:
- 5G-enabled remote ultrasound education
- Wearable smart socks for vascular disease monitoring (95.83% accuracy)
- Generative AI for low-bandwidth diagnostics
As WHO Director-General Dr. Tedros noted: "Telemedicine isn't just technology—it's health equity in action."

 Nederlands
Nederlands
 English
English
 French
French
 Deutsch
Deutsch
 Espaniol
Espaniol
 Portugese
Portugese